Plantar fasciitis is a common foot condition characterized by pain in the heel and bottom of the foot.
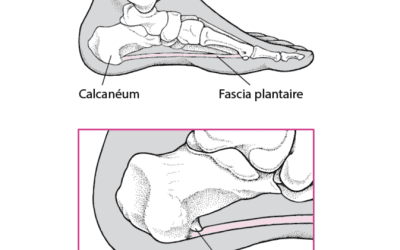
It is caused by inflammation of the plantar fascia, a band of connective tissue that connects the heel to the toes and supports the arch of the foot.
Plantar fasciitis can be caused by a variety of factors, such as overuse of the foot, inappropriate footwear, misalignment of the feet, or weight problems. Symptoms include a sharp pain in the heel or bottom of the foot, which can be particularly pronounced after a prolonged period of walking or standing.
Table of content, What is it plantar fasciitis?
Plantar fasciitis or heel spur, what’s the difference?
Plantar fasciitis and heel spur are two distinct conditions, although they are often linked.
Plantar fasciitis is an inflammation of the plantar fascia, a band of connective tissue that connects the heel bone to the toes. Symptoms include sharp pain in the heel or the arch of the foot, often felt with the first steps in the morning or after a period of rest. Plantar fasciitis can be caused by overuse, being overweight, inappropriate shoes, muscle imbalance, or poor posture.
A heel spur, on the other hand, is a bony growth that forms on the heel bone in response to excessive pulling of the plantar fascia on the bone. This excessive pulling is often caused by inflammation of the plantar fascia, as in the case of plantar fasciitis. Symptoms of a heel spur may include pain in the heel or bottom of the foot, particularly when walking or running.
In summary, plantar fasciitis is inflammation of the plantar fascia, while a heel spur is a bony growth on the heel bone that can be caused by excessive pulling of the plantar fascia. Plantar fasciitis can lead to the formation of a heel spur, but the reverse is not true.
What are the symptoms caused by plantar fasciitis?
Plantar fasciitis is characterized by a sharp and persistent pain in the heel and bottom of the foot. Symptoms can vary in intensity and duration, but they are generally more pronounced in the morning or after a prolonged period of rest or physical activity.
Common symptoms of plantar fasciitis include:
- Sharp and throbbing pain in the heel or bottom of the foot
- Foot and ankle stiffness, particularly in the morning or after a prolonged period of rest
- Burning or tingling sensation in the foot
- Swelling at the heel or bottom of the foot
- Sensitivity to touch or pressure in the affected area
- Difficulty walking normally or performing physical activities.
How is plantar fasciitis diagnosed?
The diagnosis of plantar fasciitis begins with a consultation with a healthcare professional, such as a general practitioner, podiatrist, or physiotherapist. The healthcare professional will start by collecting the patient’s medical history and will perform a physical examination to assess symptoms.
The physical examination may include:
- An examination of gait and posture
- An evaluation of sensitivity and pain on touch in the affected area
- Tests to assess the flexibility of the plantar fascia and muscles of the foot and leg
- X-rays or an ultrasound to help confirm the diagnosis and rule out other causes of foot pain.
In some cases, the healthcare professional may also recommend blood tests or more advanced imaging tests to help establish an accurate diagnosis.
What causes plantar fasciitis?
Plantar fasciitis is usually caused by overuse or excessive strain of the plantar fascia, a band of connective tissue that connects the heel to the toes and supports the arch of the foot. This strain can cause micro-tears in the plantar fascia, which can lead to inflammation and pain in the heel and bottom of the foot.
Some people are more likely to develop plantar fasciitis than others due to risk factors such as:
- Poor posture or muscle imbalance that affects walking or posture
- Inappropriate shoes that do not sufficiently support the foot
- Being overweight or obese which puts excessive pressure on the plantar fascia
- Intensive or repetitive physical activity, particularly running or activities that involve jumping or standing for long periods
- Misalignment of the feet, such as flat feet or high arches.
In some cases, plantar fasciitis can also be caused by underlying medical factors such as arthritis, neuropathy, or fibromyalgia.
How can I prevent pain associated with plantar fasciitis?
There are several preventive measures you can take to reduce the risk of developing plantar fasciitis or to prevent a relapse:
- Stretch your foot and leg muscles:
- Regular stretching exercises can help improve the flexibility and elasticity of the plantar fascia and foot and leg muscles, thereby reducing the risk of pain and strain.
- Use supportive footwear:
- Choose shoes that support the arch well and provide good cushioning to reduce pressure on the plantar fascia.
- Control your weight:
- Maintaining a healthy weight can reduce the pressure exerted on the plantar fascia and lower the risk of pain and inflammation.
- Avoid repetitive or intense activities:
- If you engage in physical activities that put a lot of stress on the feet, like running or jumping, it’s important to gradually incorporate them into your workout routine and take regular breaks to allow your muscles and tendons to recover.
- Pay attention to your posture:
- Maintain good posture and avoid positions that put excessive pressure on the feet.
- Wear orthotic insoles:
- Orthotic insoles can help correct muscle imbalances and posture that can contribute to plantar fasciitis.
By taking these preventive measures, you can reduce the risk of developing plantar fasciitis or prevent a relapse if you have already been treated for this condition.
What are some home treatments?
- There are several home treatments you can try to relieve the symptoms of plantar fasciitis:
- Stretch the plantar fascia and the foot and leg muscles regularly to improve flexibility and elasticity.
- Use a tennis ball or foam roller to gently massage the affected area and reduce pain and muscle tension.
- Apply ice to the affected area for 15 to 20 minutes at a time, several times a day, to reduce inflammation and pain.
- Use supportive shoes with good cushioning to reduce pressure on the plantar fascia.
- Avoid activities that put a lot of stress on the feet, like running or jumping, during the acute phase of pain.
- It’s important to consult a healthcare professional if symptoms persist or worsen despite these home self-care measures.
What are the medical treatments?
There are several medical treatment options for plantar fasciitis, depending on the severity of the condition:
- Orthotic insoles: Custom orthotic insoles can help correct muscle imbalances and posture that can contribute to plantar fasciitis, thus reducing pain and strain on the plantar fascia.
- Anti-inflammatory medications: Anti-inflammatory medications, such as ibuprofen or naproxen, can be prescribed to reduce pain and inflammation.
- Corticosteroid injections: Corticosteroid injections can be used to reduce inflammation and pain. However, their use should be limited as they can lead to undesirable side effects.
- Physiotherapy: Physiotherapy can be recommended to strengthen the muscles of the foot and leg, improve flexibility, and reduce pain and strain on the plantar fascia.
- Surgery: In the most severe cases, surgical intervention may be necessary to release tension on the plantar fascia. However, surgery is rarely necessary and is generally considered as a last resort.
In conclusion, plantar fasciitis
Is a common condition that can cause significant pain in the heel or arch of the foot. It can be caused by several factors, including overuse, overweight, inappropriate shoes, and muscle imbalances.
Fortunately, there are effective home and medical treatments to relieve pain and promote healing. It’s important to consult with a healthcare professional to determine the appropriate treatment based on the severity of plantar fasciitis and your medical history. Preventing this condition involves regular stretching, wearing appropriate shoes, and regular physical activity.